Will Medicaid Pay for Weight Loss Surgery?: Know Your Options: Medicaid may cover weight loss surgery if specific criteria are met. These requirements typically include a BMI over 40 or serious obesity-related health conditions.
Understanding the intricacies of Medicaid coverage for weight loss surgery is crucial for individuals seeking financial aid for this life-changing procedure. Obesity can lead to numerous health issues, and weight loss surgery, also known as bariatric surgery, has become a viable solution for many.
Medicaid, the joint federal and state program, offers coverage for those who meet the established criteria, promoting a path to healthier living for eligible low-income adults. The decision to fund such procedures is not only a benefit for those struggling with obesity but also a potential cost-saving measure for Medicaid in the long term by reducing obesity-related health complications. Therefore, it is essential to explore and confirm your eligibility for coverage with your specific state’s Medicaid program.
Eligibility Criteria For Medicaid Coverage
Understanding the requirements for Medicaid to cover weight loss surgery is important. This surgery can help improve health and well-being. For those covered by Medicaid, specific criteria must be met. The eligibility revolves around income, assets, and medical needs. Below is a guide on what Medicaid evaluates before approving this life-changing surgery.
H3 for Income and Asset AssessmentsIncome And Asset Assessments
Medicaid considers both income and assets to decide if someone qualifies. This assessment ensures aid goes to those in most need. The following points detail the financial criteria:
- Income level: It must align with the state’s Medicaid threshold.
- Assets: They must fall below a certain value, excluding essentials like home and car.
| Criteria | Details |
|---|---|
| Thresholds | Varies by state and household size |
| Asset Limit | Also varies but generally includes savings, investments, and additional properties |
Medical Necessity For Weight Loss Surgery
Medicaid requires proof that the surgery is a medical need. It is not just for cosmetic reasons. To meet this criterion, the following conditions must typically be present:
- A Body Mass Index (BMI) of 40 or higher.
- A serious health condition related to obesity, like diabetes or hypertension.
- Previous unsuccessful weight loss efforts.
A doctor’s evaluation is required. They will confirm that weight loss surgery is the best option for health improvement. Documentation of this medical opinion is crucial. Only then will Medicaid consider covering the procedure.
Types Of Weight Loss Surgeries Covered
Medicaid covers various lifesaving weight loss surgeries. Each surgery has unique benefits. We discuss common procedures Medicaid funds.
Gastric Bypass And Sleeve Gastrectomy
These surgeries reduce stomach size and food intake. Medicaid often approves them.
- Gastric Bypass: This reroutes the digestive tract. It aids significant weight loss.
- Sleeve Gastrectomy: It removes part of the stomach. It’s less invasive.
Adjustable Gastric Band Procedures
This procedure involves an adjustable band around the stomach. It controls food portions.
| Procedure | Description | Recovery Time |
|---|---|---|
| LAP-BAND | A band adjusts to limit food intake. | Short |
| Realize Band | Customizable band fits around the stomach. | Varies |
State-by-state Variation In Coverage
When it comes to weight loss surgery, Medicaid coverage varies from state to state. Each state has its own guidelines that determine eligibility and the types of procedures covered. Understanding the differences in coverage can be crucial for those considering weight loss surgery as an option for improving their health.
Different Medicaid Policies
Medicaid policies on weight loss surgery are not uniform across the United States. Some state Medicaid programs may offer comprehensive coverage that includes a variety of weight loss procedures, while others might cover only specific surgeries or none at all. It’s crucial to know the distinct requirements that may include:
- Body mass index (BMI) thresholds
- Necessity of medical clearances
- Documented history of obesity-related health conditions
- Proof of previous weight loss efforts
For instance, while one state might cover laparoscopic gastric bypass, another may restrict coverage to gastric sleeve procedures only.
Researching Your State’s Specifics
To uncover the specifics of your state’s Medicaid coverage for weight loss surgery, start by consulting official state resources. This might include:
- State Medicaid websites
- Contacts listed for state health departments
- Consultations with local Medicaid offices
It’s also wise to reach out to local clinics and hospitals that specialize in bariatric surgery. They often have knowledgeable staff familiar with state Medicaid policies. Ensure you have the most current information, as Medicaid policies can change over time. Read More …
Haven Health Scottsdale: Your Gateway to Wellness 2024
Credit: www.aslitarcanclinic.com
Pre-surgery Requirements
Understanding the steps before weight loss surgery is key. Medicaid covers weight loss surgery for eligible patients. Patients must meet specific pre-surgery requirements. This includes nutritional counseling and proof of previous weight loss efforts.
Mandatory Nutritional Counseling
Nutritional guidance is crucial before surgery. Medicaid requires patients to attend counseling sessions. Dietitians help patients prepare for post-surgery life. They teach proper eating habits and nutritional needs. These sessions ensure long-term success and safety.
Weight Loss Efforts Prior To Approval
Patients must show commitment to losing weight. Medicaid asks for documented weight loss attempts. This can be through diets, exercise programs, or clinically supervised plans. Evidence of these efforts is necessary for approval. It shows readiness for lifestyle changes post-surgery.
Below is a table summarizing the requirements:
| Requirement | Description | Duration |
|---|---|---|
| Nutritional Counseling | Guidance from a dietitian | Varies by case |
| Weight Loss Attempts | Documented efforts to lose weight | Typically 6-12 months |
To summarize, prepare with the right steps. Attend nutritional counseling. Prove your weight loss efforts. These steps are vital to secure Medicaid support for surgery.
Application Process For Medicaid Approval
Taking the step toward weight loss surgery can be life-changing. For those considering this path, understanding the Application Process for Medicaid Approval is crucial. Medicaid can potentially cover the cost of weight loss surgery, but obtaining approval requires a solid grasp of the application process. Let’s walk through the essentials, starting with gathering your documentation to smoothly navigate the Medicaid system.
Gathering Necessary Documentation
To begin, compiling the right documents is key. These documents prove your need for surgery and eligibility for coverage. You will need:
- Personal Identification: Such as a driver’s license or state ID.
- Proof of Residency: Utility bills or lease agreements work well.
- Proof of Income: Recent pay stubs, tax returns, or benefit statements.
- Medical Records: Highlighting your history with weight-related health issues.
- Physician’s Recommendation: A letter from your doctor supporting your need for surgery.
- Nutritional and Psychological Evaluations: To show you are a suitable candidate.
Navigating The Bureaucracy
Understanding Medicaid’s procedures ensures your application won’t hit a snag. Here’s how to stay on track:
- Contact your state’s Medicaid office. Get specifics on the process.
- Submit your application. Include all necessary documentation.
- Track your application. Follow up regularly for updates.
- Respond promptly. Provide any additional information if requested.
- Appeal if needed. Don’t get discouraged by initial denials; appeal and present your case.
Patience is key throughout this process. Ensure every step is meticulously followed. Your path to a healthier life is waiting, and Medicaid may just be the support you need to reach it.
Read More …
Who Pays Health Insurance While on Long-Term Disability: Unveiled!

Credit: www.youtube.com
Appealing A Medicaid Denial
Facing a Medicaid Denial for weight loss surgery can be disheartening. Yet, there’s hope. An appealing journey often leads to a successful overturn of decisions. This section guides through appealing a Medicaid denial.
Understanding The Appeals Process
Medicaid offers an appeals process for denials of weight loss surgery coverage. Know the steps:
- Request an appeal in writing within the given time frame.
- Prepare documentation: medical records, doctor’s notes, and any evidence supporting the necessity of surgery.
- Undergo a fair hearing where you can present your case to a judge or an appeals board.
Adhere strictly to Medicaid deadlines. Missing them could waive your right to appeal. Keep detailed records of all communication.
When To Seek Legal Help
While the appeals process is user-friendly, complex cases require legal assistance. Consider seeking legal help if:
- Your initial appeal was unsuccessful.
- You don’t understand the denial reasons.
- Deadlines seem confusing or are fast approaching.
Legal experts specialize in Medicaid appeals. They know how to navigate the system effectively. Reach out promptly for the best chance at a positive outcome.
Alternatives If Medicaid Denies Coverage
If Medicaid declines coverage for weight loss surgery, you’re not at a dead end. Multiple pathways exist to help manage the financial burden of this life-changing procedure. Let’s explore some viable alternatives that can provide the necessary funds.
Private Insurance Plans
Private insurance may cover what Medicaid won’t. Always verify your policy’s specifics. Coverage often hinges on certain criteria, like a doctor’s recommendation. Different insurers offer varied benefits, so research and compare plans thoroughly.
Payment Plans And Financing Options
Healthcare facilities frequently offer payment plans, allowing for gradual repayment. Facilities break down hefty surgery costs into manageable monthly payments. Additionally, medical financing companies specialize in healthcare-related loans. These companies offer flexible repayment terms to suit different budgets. It’s crucial to shop around for the best rates and terms that align with your financial situation. Aim for plans without prepayment penalties and reasonable interest rates.
Lifestyle Changes Post-surgery
Embarking on a weight loss surgery journey with Medicaid doesn’t end in the operating room. Successful long-term results hinge on making significant lifestyle adjustments. Adapting to these changes is vital for maintaining health, optimizing surgery benefits, and preventing complications. Let’s explore the essential post-operative lifestyle transformations.
Dietary Adjustments
After weight loss surgery, your stomach’s size is much smaller. You’ll need to eat much less and focus on highly nutritious foods.
- Protein-rich foods aid in healing and maintenance of muscle.
- Vegetables and fruits become key for their vitamins and fiber.
- Small, regular meals help the body to adapt.
- Sugary, high-fat, and empty-calorie foods are avoided.
Understanding your new dietary needs is crucial. A qualified dietitian can help create a tailored plan.
Ongoing Medical Support
Your journey doesn’t stop at the procedure. Ongoing medical support ensures success and safeguards your health.
- Regular check-ups monitor your progress and health status.
- Blood tests may be necessary to check nutrient levels.
- A psychologist can support mental and emotional adaptations.
- Support groups provide peer encouragement and tips.
Combining these changes with physical activity cements the foundation for a healthier future. Your care team can help every step of the way.
Success Stories And Motivation
Discovering the possibility of Medicaid covering weight loss surgery can spark hope for many. But it’s the personal triumphs of those who’ve walked this path that truly inspire. Here, we dive into the success stories that motivate and guide future candidates on their weight loss journey through Medicaid.
Real-life Experiences
Inspirational tales of weight loss surgery can often be a tipping point for decision-making. Across the country, countless individuals have transformed their lives after undergoing bariatric surgery funded by Medicaid.
- Stories underscore the challenges, the milestones, and the victories.
- They capture the life-changing moments that follow successful operations.
- Many share the benefits of surgery beyond weight loss, like improved health and well-being.
Staying Strong Through The Medicaid Process
Navigating the Medicaid system for weight loss surgery eligibility may seem daunting. But with determination and the right support, embarking on this journey is absolutely achievable.
- Meet with your primary care physician: Establish the medical necessity of your surgery.
- Gather required documentation: Proof of previous weight loss attempts is vital.
- Stay persistent: Continuous follow-ups with Medicaid could be the key to approval.
Those who have persisted share feelings of empowerment and resilience, urging others to not give up on their health goals.
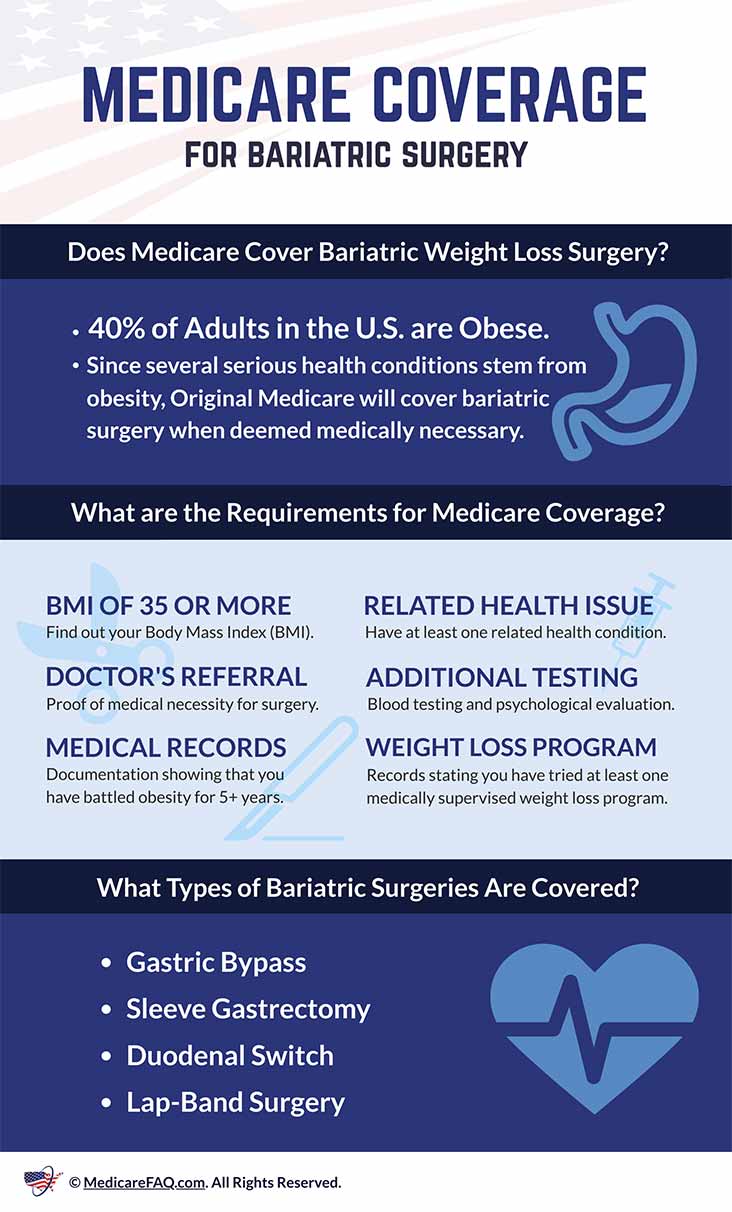
Credit: www.medicarefaq.com
Frequently Asked Questions
How Do You Get Approved For Weight Loss Surgery?
To get approved for weight loss surgery, consult with a healthcare provider, meet body mass index (BMI) qualifications, undergo a psychological evaluation, complete a medically supervised weight loss program, and secure insurance or financial approval.
How Long Does It Take Medicare To Approve Bariatric Surgery?
Medicare approval for bariatric surgery typically takes 1-2 months after completing necessary prerequisites and documentation. Always consult with your provider for specific timelines.
Does Medicaid Cover Weight Loss Surgery In Florida?
Yes, Medicaid covers weight loss surgery in Florida, but patients must meet specific eligibility criteria and obtain prior authorization.
How Do People Afford Weight Loss Surgery?
People afford weight loss surgery through insurance coverage, payment plans, medical loans, savings, or financial assistance programs. Some also opt for surgery abroad where costs may be lower.
Conclusion
Navigating Medicaid coverage for weight loss surgery can be complex. Eligibility hinges on state-specific criteria and medical necessity. Consulting with a specialist helps clarify your options. If qualified, Medicaid’s support can be a transformative step towards a healthier future. Always verify your coverage to ensure a smooth journey to wellness.