Blue Cross Blue Shield coverage for Wegovy varies by plan and location. Contact your specific BCBS provider to confirm if they include Wegovy for weight loss.
Blue Cross Blue Shield (BCBS) is a federation of 35 separate United States health insurance organizations that provide health insurance to over 106 million Americans. As a popular medication for weight loss, Wegovy has garnered attention from those looking to manage obesity through pharmacological means.
Navigating insurance coverage can be complex, and for those with a Blue Cross Blue Shield plan, the specifics of your coverage for prescription medications like Wegovy depend on your individual policy details, the state you reside in, and the policy’s formulary. Verifying your coverage directly with your BCBS provider ensures accurate information. This can help manage your healthcare expenses and plan your weight loss strategy effectively.
Introduction To Wegovy And Weight Loss
The search for effective weight loss solutions has led to the creation of Wegovy. Wegovy is a prescription medication designed to assist with weight loss. It targets individuals who struggle with obesity. Let’s explore the impact Wegovy has in the realm of weight management and healthcare coverage.
Wegovy’s Role In Treating Obesity
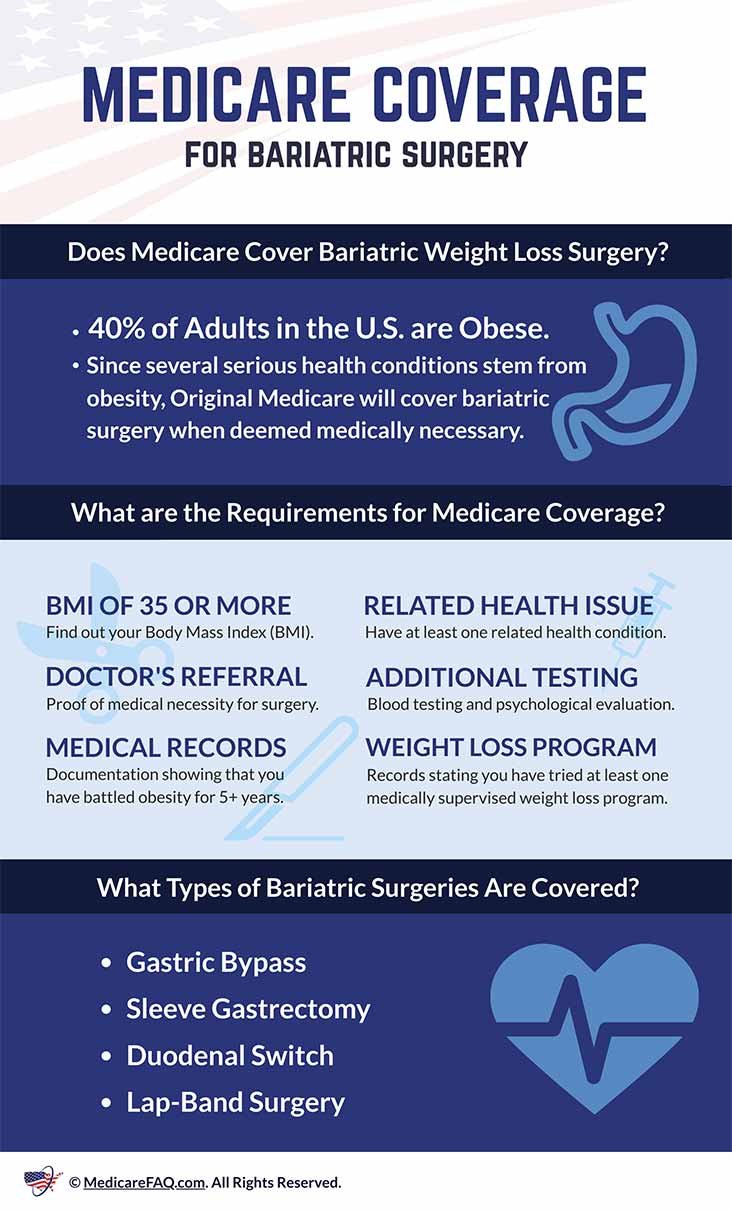
Wegovy is a game-changer in the battle against obesity. This medication works by mimicking a hormone that targets areas of the brain regulating appetite and food intake. Approved for those with a body mass index (BMI) over 30, or over 27 with at least one weight-related condition, its role is crucial. By aiding weight loss, Wegovy can reduce the risk of health issues linked to obesity, like heart disease and diabetes.
The Rising Demand For Weight Loss Medications
Obesity rates are soaring globally. This creates a high demand for safe and effective weight loss medications. People seek treatments that deliver results while minimizing health risks. As lifestyles become more sedentary and calorie-rich diets more common, weight loss medications like Wegovy are increasingly sought after. They are seen as tools to help achieve healthier weights and improve overall wellness.
Navigating Insurance Coverage
Exploring the ins and outs of insurance coverage can feel like a maze. Specifically, when discussing Wegovy for weight loss, questions arise. Does Blue Cross Blue Shield provide coverage? This section walks you through the healthcare insurance landscape to find clear answers.
The Basics Of Health Insurance
Understanding your health insurance is the first step. Health plans differ in coverage and costs. Most include premiums, deductibles, and copays. Prescription coverage is key for medications like Wegovy. Check your plan’s summary of benefits before proceeding.
Coverage Variables
Blue Cross Blue Shield’s coverage for Wegovy varies. Factors include plan type, location, and medical necessity. Some plans offer weight loss medication coverage, others don’t. Below is a checklist to determine if you’re covered:
- Review your policy: Find the prescription drugs section.
- Verify formulary status: Does Wegovy appear on the list?
- Ask your doctor to justify medical necessity.
- Consider prior authorization: It may be required for Wegovy.
- Explore alternative coverage options if denied.
Remember, persistence is key.
Blue Cross Blue Shield: An Overview
Blue Cross Blue Shield (BCBS) stands as a trusted name in health insurance. Covering millions of Americans, BCBS has a history of providing diverse healthcare plans. Individuals and families trust BCBS for their healthcare needs. This includes weight loss treatments like Wegovy. Let’s delve into the company’s profile and the range of health plans they offer.
Company Profile
The Blue Cross Blue Shield Association boasts a vast network of companies. The Association began in the 1920s. It now serves all 50 states. Its member companies work independently.
- Founded: 1929
- Headquarters: Chicago, IL
- Network: Over 90% of doctors and hospitals nationwide
- Mission: Provide affordable healthcare
Range Of Health Plans
BCBS offers various plans. They cater to different health needs and budgets.
| Plan Type | Features |
|---|---|
| HMO | Cost-effective, In-network doctors |
| PPO | Flexibility, Out-of-network coverage |
| EPO | Balance of HMO and PPO, Selected network |
| Medicare/Medicaid | Federal plans, Seniors and low-income individuals |
Each plan has its own coverage details. Members can choose the best plan for their needs.

Credit: jetmedicaltourism.com
Insurance Coverage For Prescription Drugs
Understanding insurance coverage for prescription drugs is vital. Each plan has its rules. Blue Cross Blue Shield (BCBS) provides health insurance to many. They cover various medications. Let’s explore if BCBS covers Wegovy for weight loss.
Standard Criteria For Medication Coverage
Insurers use criteria to decide coverage. This ensures drugs are safe and effective. BCBS looks at:
- Drug safety reviews
- Clinical effectiveness
- Cost-effectiveness
The medication must meet these points for approval.
Formulary Lists And Their Importance
Formulary lists show covered drugs. BCBS updates this list often. Check this list to see if Wegovy is covered. It details:
- Drug tiers
- Copayment amounts
- Coverage restrictions
Find your plan’s formulary list online. Contact BCBS for the most current information.
Evaluating Coverage For Wegovy
When considering Wegovy for weight loss, understanding your insurance coverage is crucial. Blue Cross Blue Shield (BCBS) policy holders may wonder if their plan covers this medication. This post guides you through evaluating whether BCBS provides coverage for Wegovy and how to verify your benefits.
Specifics Of Bcbs Drug Coverage
BCBS offers various insurance plans, each with different levels of prescription coverage. The specifics can include:
- Formulary inclusion – Whether Wegovy is on your plan’s list of covered drugs.
- Tier placement – The cost-sharing tier Wegovy falls under, which affects your out-of-pocket costs.
- Prior authorization requirements – A possible necessity for approval from BCBS before coverage is available.
- Quantity limits – A cap on the amount of Wegovy you can receive in a certain time frame.
Verification Process For Medication Coverage
To verify if your BCBS plan covers Wegovy, follow these steps:
- Review your insurance card or member handbook for member services contact information.
- Call member services and provide your policy number.
- Request information specifically about Wegovy coverage under your plan.
- Ask about any prior authorization, documentation, or additional steps needed to secure coverage.
Remember, coverage may vary by state and individual policy. Always double-check with BCBS directly for the most accurate information.
Factors Influencing Bcbs Coverage Decisions
Understanding insurance coverage can be complicated. Many people wonder about Blue Cross Blue Shield (BCBS) coverage for treatments like Wegovy for weight loss. BCBS considers several factors before deciding if they will cover a weight loss medication. Let’s discuss these factors.
Clinical Guidelines And Weight Loss Treatments
BCBS follows strict clinical guidelines to ensure the safety and effectiveness of weight loss treatments. These guidelines include:
- Evidence of benefits from well-conducted clinical trials.
- Patient’s health conditions and medical history review.
- Expert recommendations from medical societies.
These checkpoints help BCBS to decide if Wegovy is the right choice for their members.
Cost-benefit Analysis Of Weight Loss Medications
Cost is a major factor for insurance companies. BCBS performs a cost-benefit analysis to assess:
| Cost Element | Benefit Element |
|---|---|
| Price of medication | Improvement in health |
| Long-term healthcare savings | Reduction in weight-related issues |
They compare the medication’s cost against potential healthcare savings and health benefits for the patient. If the benefits outweigh the costs, BCBS may cover Wegovy for weight loss.
Case Studies And Precedents
Welcome to our exploration of how Blue Cross Blue Shield insurance might cover Wegovy for weight loss. We dive into real-life experiences. We learn from them. Below, you’ll find true stories of people dealing with insurance. Plus, the tasks they faced in getting coverage for Wegovy.
Previous Authorization Success Stories
Every victory starts with a story. Here we celebrate the wins. Patients who sought Wegovy for weight loss found an ally in Blue Cross Blue Shield. A closer look:
- Jane’s Journey: After many tries, her doctor’s persistence paid off. BCBS approved her treatment.
- Alex’s Achievement: With clear medical need, Alex got the green light. BCBS saw Wegovy as essential.
- Emma’s Experience: She shared her story online. Community support helped. Her request got accepted.
Challenges In Obtaining Coverage For Wegovy
Not all attempts are smooth. Patients often hit roadblocks. Each case teaches us something new. Key lessons:
- Documentation: Without it, denials happen. Effort in record-keeping can pave ways for approval.
- Policy Details: Understanding what’s covered is vital. Sometimes, it’s about decoding the fine print.
- Persistence: Don’t give up. Some found success after multiple tries. Keep pushing.
These experiences serve as guides. They help us navigate the complex world of insurance coverage for Wegovy.

Credit: www.singlecare.com
Navigating Challenges With Insurance
Navigating the maze of insurance coverage can be daunting. When considering a medication like Wegovy for weight loss, understanding what Blue Cross Blue Shield covers is crucial. Insurance policies vary, and approvals for treatment can hinge on specific criteria set by the insurer. Here, we will delve into strategies that can help secure the coverage you need.
Strategies To Advocate For Coverage
- Review your policy: Understanding the inclusions and exclusions of your insurance plan is the first step.
- Consult your doctor: A health professional’s recommendation can be persuasive. They can document your need for Wegovy.
- Gather evidence: Clinical studies and evidence of Wegovy’s efficacy can support your case.
- Prepare a letter of medical necessity: This formal request outlines why Wegovy is essential for your health.
- Contact customer service: Speaking directly with Blue Cross Blue Shield representatives can provide additional guidance.
Appealing Insurance Decisions
If initially denied, don’t lose hope. An appeal can overturn the decision. Start this process guided by the steps below:
- Understand the denial: Identify the reason Blue Cross Blue Shield may have declined coverage for Wegovy.
- Review the appeals process: Each insurer has a set appeals protocol. Follow it thoroughly.
- Submit documentation: Provide comprehensive information, including medical records and your doctor’s support.
- Stay persistent: Follow up regularly and keep track of all communications for reference.
The Road Ahead For Obesity Treatment Coverage
Obesity is a growing concern worldwide. Effective treatments like Wegovy offer hope. Insurance coverage plays a pivotal role. Today, we’re exploring future coverage prospects for obesity treatments. We’ll delve into what that means for patients seeking Wegovy.
Emerging Trends In Health Insurance
Health insurance is evolving. Insurers recognize obesity as a serious health issue. Policy updates reflect this change. We see more plans covering weight loss treatments. Patients gain easier access to life-changing medications.
- Preventive care focus grows within insurance policies.
- Companies acknowledge the cost-saving benefits of obesity treatment.
- Comprehensive coverage includes medications like Wegovy.
The Future Of Wegovy And Similar Medications
Wegovy has shown impressive results in weight loss. Insurers are taking notice. Future coverage looks promising. Plans may soon extend to include Wegovy routinely. This can open doors for patients struggling with weight loss.
| Year | Coverage Trend |
|---|---|
| Current | Limited coverage under certain plans |
| Near Future | Wegovy inclusion in more insurance plans |
| Long-Term | Standard obesity treatment coverage |
Research fuels innovation. New medications like Wegovy enter the market. Interest spikes in effective weight loss solutions. As results become more evident, insurance companies will likely adjust coverage accordingly.

Credit: medium.com
Frequently Asked Questions
What Insurance Companies Cover Wegovy For Weight Loss?
Coverage for Wegovy varies by insurance company and individual policy. Check with providers like Aetna, Cigna, and UnitedHealthcare, but confirm specifics with your insurer. Always review your plan benefits for the latest information on weight loss medication coverage.
What Are The Requirements To Qualify For Wegovy?
To qualify for Wegovy, you must have a body mass index (BMI) of 30 or higher, or 27 or higher with at least one weight-related condition, such as type 2 diabetes, high blood pressure, or high cholesterol. A doctor’s prescription is required.
How Do You Get $25 Wegovy?
To get $25 Wegovy, secure a valid prescription, visit the Wegovy Savings Card website, and sign up for the coupon program. Eligibility criteria apply.
Does Anthem Bcbs Cover Wegovy For Weight Loss?
Anthem BCBS may cover Wegovy for weight loss based on your specific plan and medical necessity. Verify coverage directly with Anthem and consult your doctor for eligibility.
Conclusion
Understanding insurance coverage for weight loss medications can be complex. Blue Cross Blue Shield policies vary widely, impacting Wegovy coverage. Consult your plan and health provider for personalized info. Emphasize the importance of checking individual benefits for clarity on this topic with Blue Cross Blue Shield.