Medicaid does cover weight loss surgery, but eligibility and coverage vary by state. Coverage depends on meeting certain criteria, including medical necessity.
Navigating the intricate domain of Medicaid coverage for weight loss surgery can be daunting for those seeking a solution to obesity-related health issues. The process is dictated by specific guidelines that define eligibility and preoperative requirements. As obesity rates rise, the demand for weight loss surgery increases, prompting many to explore their insurance options.
Medicaid, as a state and federally funded program, offers a lifeline to those who qualify—understanding the prerequisites and steps involved is crucial for a successful journey towards a healthier life. Eligible recipients may find that weight loss procedures, including gastric bypass and sleeve gastrectomy, can be a covered benefit, providing them with access to potentially life-changing operations.
Credit: www.aslitarcanclinic.com
Introduction To Medicaid And Weight Loss Surgery
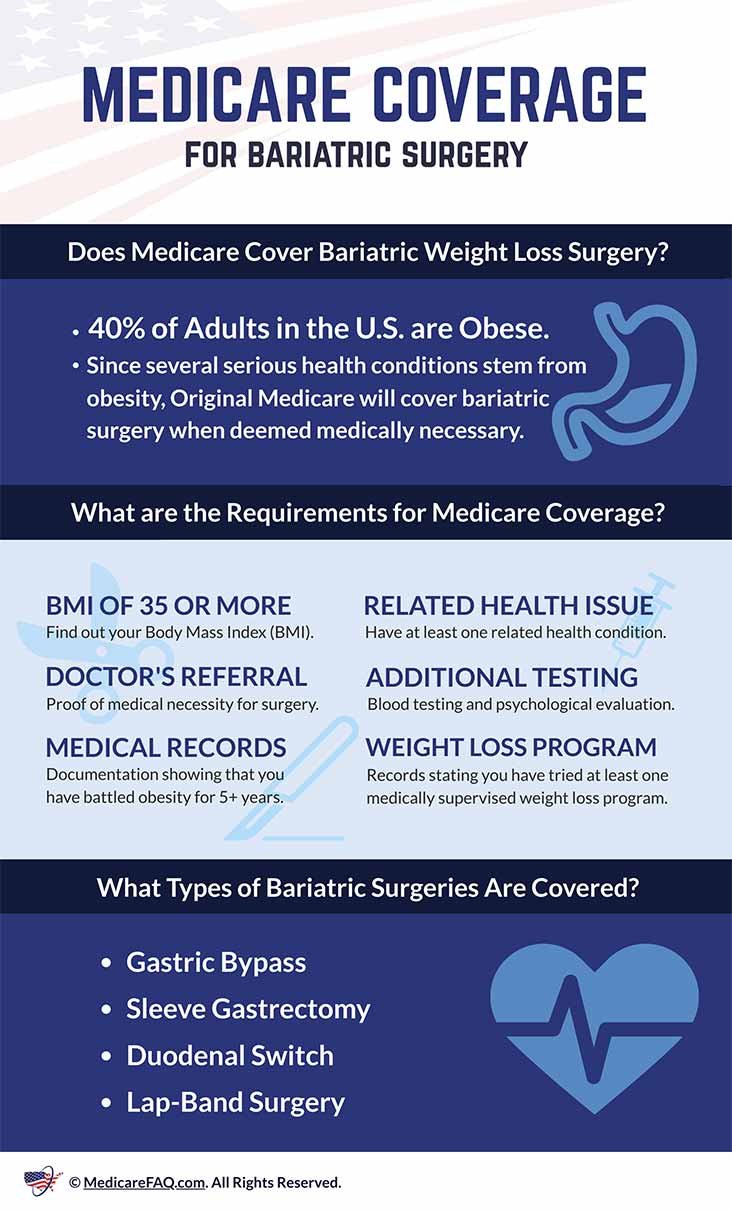
Understanding the support Medicaid provides for weight loss surgery is vital in the fight against obesity. As rates of obesity climb, more individuals seek medical interventions to improve their health. Medicaid, a joint federal and state program, helps with medical costs for some people with limited income and resources. It also offers benefits not normally covered by Medicare, including weight loss surgery for qualifying candidates.
The Rising Epidemic Of Obesity
Obesity has become a critical health crisis affecting millions in the United States. It leads to severe health complications like diabetes, heart disease, and hypertension. Recognizing the gravity of the situation, Medicaid has extended its coverage to include treatments that cater to obesity-related conditions.
Bariatric Procedures: A Brief Overview
Weight loss surgery, or bariatric surgery, includes different procedures to help reduce weight and improve health. The primary surgeries covered typically include:
- Gastric Bypass: Reduces the stomach size and bypasses part of the small intestine.
- Sleeve Gastrectomy: Removes a large part of the stomach, limiting food intake.
- Adjustable Gastric Band: Places a band around the top of the stomach to create a small pouch.
Eligibility for these procedures under Medicaid varies by state and requires meeting certain criteria, including morbid obesity and previous unsuccessful weight management efforts.
Eligibility Criteria For Medicaid Coverage
Medicaid’s coverage for weight loss surgery can be the turning point in a journey towards health. Understanding the eligibility criteria is crucial. Medicaid often has specific requirements that individuals must meet to qualify for surgery. This includes particular health conditions and Body Mass Index (BMI) thresholds.
Qualifying Conditions For Weight Loss Surgery
Medicaid looks for certain medical conditions to approve weight loss surgery. These conditions go beyond wanting to shed excess weight. Immediately below are typical qualifying conditions:
- Type 2 diabetes
- Obstructive sleep apnea
- Heart disease
- Hypertension
Also, a documented history of unsuccessful weight management may be necessary. Each state may have variations in qualifying conditions. Check with your local Medicaid program.
Understanding Body Mass Index (bmi) Requirements
The Body Mass Index (BMI) measures body fat based on height and weight. For Medicaid to cover weight loss surgery, an individual’s BMI plays a critical role. The following are standard BMI requirements:
| BMI Value | Status | Medicaid Coverage |
|---|---|---|
| 40 or above | Severely obese | Generally covered |
| 35 to 39.9 | Obese with conditions | Possible coverage with additional health conditions |
These BMI figures ensure that the surgery goes to those in significant need. Again, requirements may vary, so it’s essential to verify with your state’s Medicaid office.
State-specific Variations In Coverage
Many in the United States struggle with obesity and its health complications. Medicaid coverage for weight loss surgery can offer hope, yet it varies by state. Understanding the breadth of Medicaid’s assistance requires diving into these state-specific variations.
How Coverage Differs Across The Us
States tailor Medicaid programs under federal guidelines. This results in different coverage options nationwide. Here are factors influencing variability:
- Type of weight loss surgeries covered: Some states may only cover certain procedures.
- Eligibility requirements: Criteria such as BMI thresholds can differ.
- Pre-surgery conditions: Such as mandatory participation in a weight loss program.
Researching Your State’s Medicaid Policy
Staying informed about your state’s Medicaid policy is crucial. Explore these steps to research:
- Contact your state’s Medicaid office. They can provide up-to-date information.
- Consult a healthcare provider. They often understand how to navigate these policies.
- Review the official Medicaid website for your state. It offers details on coverage specifics.
- Reach out to support groups or individuals who have undergone weight loss surgery through Medicaid in your state.

Credit: jetmedicaltourism.com
Types Of Bariatric Surgery Covered
Facing the challenge of obesity, many turn to bariatric surgery for a solution. Medicaid, as a provider of health coverage for millions, recognizes the importance of this life-changing surgery. But what types of bariatric procedures does Medicaid cover?
Most Common Procedures Approved By Medicaid
Medicaid coverage extends to several weight loss surgeries. Each procedure has its own set of criteria and purposes, aiming to reduce food intake and promote weight loss. The following are commonly accepted by Medicaid:
- Gastric bypass – where the stomach is divided into a small upper pouch and a larger lower remnant, and the small intestine is rearranged to connect to both.
- Sleeve gastrectomy – involves removing a portion of the stomach, creating a smaller, banana-shaped stomach.
- Adjustable gastric band – places a band around the upper part of the stomach; it’s less invasive and adjustable.
All these procedures help limit food consumption and promote a healthier lifestyle.
Restrictions And Exclusions To Know About
While Medicaid covers several surgeries, there are stipulations. Requirements often include a body mass index (BMI) over 40 or a lower BMI with serious obesity-related conditions. Patients must also typically demonstrate previous unsuccessful weight loss attempts.
| Procedure | Requirement |
|---|---|
| Gastric Bypass | BMI > 40 or > 35 with conditions |
| Sleeve Gastrectomy | BMI > 40 or > 35 with conditions |
| Adjustable Gastric Band | Previous weight loss attempts |
Restrictions may include age limits and psychological evaluation. Medicaid might also require participation in a medically supervised weight loss program before approving surgery. Understanding these restrictions is crucial before planning a weight loss surgery journey.
The Pre-approval Process
The Pre-Approval Process begins long before the surgery itself. This vital step determines if Medicaid will cover your weight loss surgery. Understanding this process is crucial. Without approval, patients may face the full financial burden. The journey to approval consists of several key steps, all designed to prove the necessity of surgery for your health.
Steps To Getting Your Surgery Approved
Medicaid has specific criteria for weight loss surgery coverage. Follow these steps to boost your approval chances:
- Check Medicaid’s requirements in your state.
- Consult with your primary care doctor.
- Get a referral to a bariatric surgeon.
- Attend a mandatory information session.
- Complete all required evaluations.
- Submit your application with necessary documentation.
Documentation: Proving The Medical Necessity
Gathering the right documents is the backbone of the pre-approval process. Medical history, past weight loss attempts, and current health status must be documented. The following items help establish the medical need:
- Medical records: showing obesity-related health problems.
- Weight history: often includes charts or logs from previous diets.
- Psychological evaluation: to ensure mental readiness for surgery.
- Nutritional assessment: from a registered dietitian.
- Letter of medical necessity: your surgeon explains why surgery is essential.
The Role Of Health Providers In The Approval Process
Navigating the qualifications for Medicaid coverage on weight loss surgery can feel complex. Health providers play a pivotal role in the approval process, guiding patients through the necessary steps to obtain coverage. Understanding the intricacies ensures a smoother journey toward a healthier future.
Working With Your Doctor For Coverage
Communication with your doctor is the first step. Doctors assess eligibility for weight loss surgery under Medicaid. They also compile the needed medical documentation. This evidence shows that surgery is not just wanted but medically necessary. Patients must often show prior weight loss efforts through documented programs. This could include diet plans, exercise routines, and other non-surgical approaches.
Medical histories and current health status are significant factors. The doctor’s records must reflect a clear need for the surgery to combat obesity-related health issues. Conditions might include diabetes, sleep apnea, or high blood pressure. Your doctor will determine if your case meets the Medicaid requirements for weight loss procedures.
Why Support From Healthcare Professionals Is Crucial
Healthcare providers not only diagnose and treat but also advocate for their patients. Their support is often the deciding factor in approval for surgery. They liaise with Medicaid, presenting the case. Documentation from different healthcare professionals might be necessary. This can include nurses, dietitians, and therapists. Each offers a critical perspective on the patient’s health and the surgery’s potential benefits.
- Provides clinical evidence to support the need for surgery
- Ensures requirements are met and clearly documented
- Helps navigate complex Medicaid policies and guidelines
Endorsements from your healthcare team are essential. They affirm the surgery as a healthcare necessity. Medicaid takes these professional opinions seriously in their assessment. A well-documented application increases chances for coverage.
After Approval: Preparing For Surgery
Getting the green light for Medicaid to cover weight loss surgery is a major step. Once approved, your focus shifts to getting ready for the procedure. Preparation is key to make sure everything goes smoothly.
Lifestyle Changes Required Before The Procedure
Adopting new habits is crucial before surgery. Doctors often ask patients to:
- Stop smoking to improve recovery.
- Reduce calorie intake to shrink the liver and lower surgery risks.
- Start a routine of physical activity to get fit for the procedure.
- Begin taking vitamin supplements as directed by your healthcare provider.
Meeting with a nutritionist can help set up a pre-surgery diet plan. Sticking to it is vital for success.
Understanding The Risks And Post-surgery Care
Learning about the risks is part of your journey. Potential complications might include:
| Risk | Description |
|---|---|
| Infection | Germs might cause harm at surgery sites. |
| Blood clots | Clots can form and block blood flow. |
| Leaks | Stomach contents might leak and cause infection. |
After surgery, care includes:
- Taking medicine as directed.
- Eating liquid foods and slowly moving to solids.
- Staying hydrated but not drinking with meals.
- Keeping up with follow-up appointments.
Remember, a support system of family, friends, and support groups will help you greatly. Keep in touch with them and your healthcare team.

Credit: jetmedicaltourism.com
Case Studies And Success Stories
Exploring the journeys of individuals who’ve undertaken weight loss surgery with Medicaid can inspire and inform others. These stories are not just about shedding pounds but about dramatic lifestyle changes and improved health outcomes.
Real-life Experiences With Medicaid Coverage
Many wonder if Medicaid really opens the door to weight loss surgery. To answer this, let’s delve into real stories.
| Patient | State | Procedure | Outcome |
|---|---|---|---|
| Emily R. | Ohio | Gastric Bypass | Approved after 6 months |
| Mark L. | California | Sleeve Gastrectomy | Covered with dietitian visits |
| Susan T. | Florida | Lap-Band | Needed BMI documentation |
These individuals battled obesity and achieved remarkable success. Medicaid covered their surgeries after specific criteria were met.
Impact Of Surgery On Patients’ Lives
- Improved Health: Patients report reduced obesity-related illnesses.
- Increased Mobility: Daily tasks become easier as mobility improves.
- Enhanced Self-Esteem: With weight loss, self-confidence soars.
Stories like that of John P. from New York, who lost 150 pounds after Medicaid-approved bariatric surgery, illustrate life-altering changes. John shares that the procedure curbed his diabetes and hypertension.
Similar testimony comes from Lisa G. from Texas. She experienced a 100-pound weight loss. Lisa’s success led to better sleep and diminished joint pain.
Potential Obstacles And How To Overcome Them
Seeking Medicaid coverage for weight loss surgery can feel like navigating a maze. The process involves strict criteria and extensive documentation. Knowing potential setbacks and solutions can streamline your journey. Let’s explore how to deal with common roadblocks.
Common Denial Reasons
- Insufficient medical documentation: Ensure all records reflect the medical necessity of the surgery.
- Lack of compliance with program requirements: Attend all required consultations and diet programs.
- Procedure not deemed medically necessary: Get a detailed letter from your surgeon explaining why the surgery is essential for your health.
Appeals Process
If Medicaid denies your weight loss surgery claim, don’t lose hope. An appeal might reverse the decision. Follow these steps:
- Read the denial letter carefully. Understand why they denied your request.
- Gather more evidence. This might include medical records or letters from your doctors.
- File the appeal within the given timeframe. Time is critical, so act quickly.
- Prepare for a hearing. State your case effectively with all supporting documents.
Resource Guide: Help Beyond Medicaid
Medicaid isn’t the only option. Here are other resources:
| Resource | Description | Contact |
|---|---|---|
| Hospital Charity Programs | Some hospitals offer financial assistance for surgeries. | Check with local hospitals. |
| Nonprofit Organizations | Groups may fund surgeries for qualifying individuals. | Search for weight loss surgery grants. |
| Payment Plans | Clinics may offer payment options to spread out the cost. | Discuss with your surgery center. |
Always stay persistent and informed. Help exists beyond Medicaid.
Conclusion: Empowering Patients Through Information
Unraveling the complexities of healthcare can lead to powerful choices for individuals. Knowledge about Medicaid coverage for weight loss surgery is no exception. This guide aims to bolster patient confidence. It equips you with essential information to navigate this healthcare journey.
Taking Control Of Your Health Journey
Understanding your Medicaid benefits is the first step. It puts the power back in your hands. Knowing if weight loss surgery is an option can be life-changing. Remember, eligibility details can differ from state to state. Always check with your local Medicaid office for the most accurate information.
Create a personal health file. Within it, document your medical history, BMI, and any weight-related issues. A strong case helps when discussing options with your healthcare provider.
Be proactive with your health team. Discuss your weight loss goals. Ask about surgery types covered, such as gastric bypass or sleeve gastrectomy.
The Importance Of Continued Advocacy
Navigating Medicaid requires perseverance. Partnerships with doctors, dietitians, and support groups contribute to success. Advocate for your health rights.
Stay informed. Health policies can change. Regular updates on Medicaid coverage keep you one step ahead.
Empower others. Share your journey. Your story may inspire and guide others in similar situations.
Frequently Asked Questions
How Do You Get Approved For Weight Loss Surgery?
To get approved for weight loss surgery, meet the BMI requirements, obtain a physician’s evaluation, complete a psychological assessment, show a history of weight loss efforts, and secure insurance or payment plans.
How Do People Afford Weight Loss Surgery?
People afford weight loss surgery through various means including health insurance coverage, medical loans, payment plans from surgical centers, or personal savings. Some also explore options like crowdfunding or financial assistance from non-profit organizations.
Does Insurance Ever Cover Weight Loss Surgery?
Yes, insurance often covers weight loss surgery if it’s deemed medically necessary and specific criteria are met. Always check with your provider for coverage details.
How Much Do You Have To Weigh To Do Gastric Bypass?
Candidates for gastric bypass surgery typically need a BMI of 40 or higher. Alternatively, a BMI of 35 may qualify with obesity-related health conditions.
Conclusion
Understanding Medicaid’s coverage for weight loss surgery is essential for anyone considering this life-changing procedure. Eligibility requirements vary by state, and pre-approval steps are crucial. The journey to better health is significant, and while Medicaid may be a pathway for some, it’s important to explore all possible options and guidelines.
Stay informed and take the next step towards a healthier future with confidence.