Does Aetna Cover Ozempic for Weight Loss? Unveiled Facts!: Aetna’s coverage for Ozempic as a weight loss treatment varies based on individual policy terms. It’s essential to consult your specific plan for eligibility and coverage details.
Aetna is a prominent health insurance provider that offers a range of coverages for medications prescribed for various conditions. As obesity becomes a growing concern, many patients seek treatments like Ozempic, a medication initially approved for managing type 2 diabetes but also shown to aid in weight loss.
Coverage for such medications can be complex, and insurers like Aetna evaluate claims based on medical necessity and the terms set out in their health plans. Before starting Ozempic for weight loss, Aetna subscribers should verify their policy’s benefits and any prior authorization requirements. Understanding your insurance coverage is crucial for accessing treatments like Ozempic without unexpected expenses.

Credit: www.forbes.com
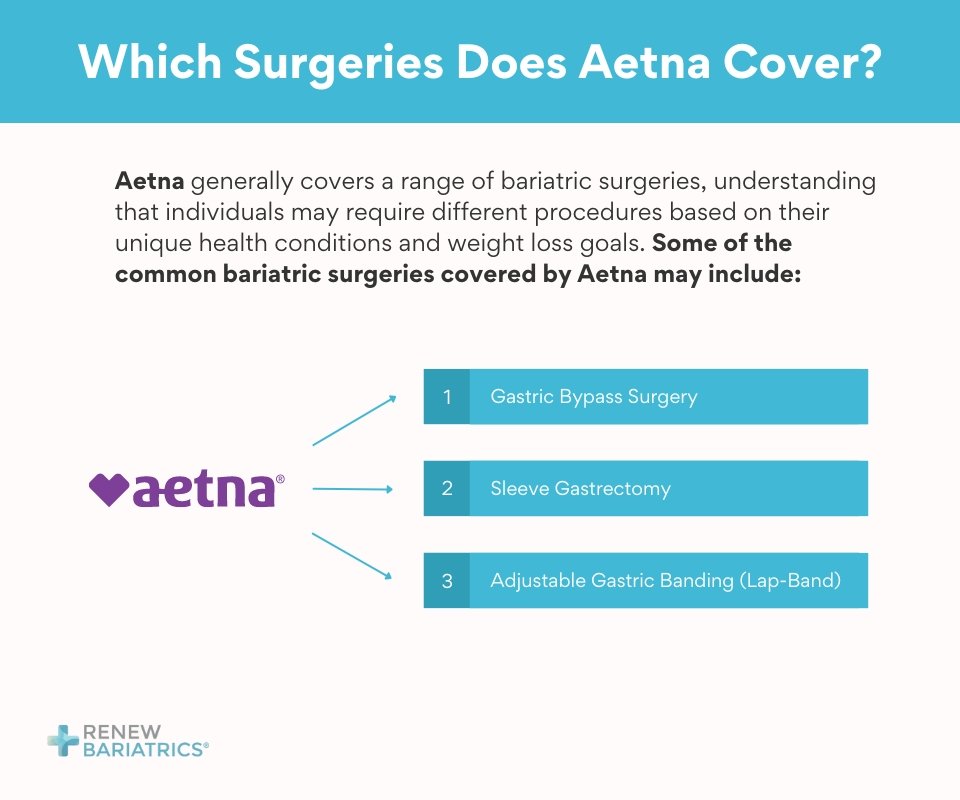
Aetna’s Stance On Obesity
Obesity is not just a number on a scale; it’s a health crisis. Aetna understands this. They view obesity as a complex, chronic disease. As a leading health insurance provider, Aetna recognizes the need for effective treatment options. This includes prescription medications like Ozempic, commonly used for weight management.
Recognizing Obesity As A Medical Condition
Medical experts classify obesity as a disease. This disease can lead to diabetes, heart disease, and more. Aetna follows this view. They seek to provide support for those dealing with the health challenges obesity brings.
Insurance Coverage For Weight Management
Managing weight is key to combating obesity. Coverage varies with each Aetna plan. Policyholders should check their plan’s details. A quick review can reveal if Aetna covers Ozempic for weight loss.
| Medication | Coverage under Aetna | Notes |
|---|---|---|
| Ozempic | Depends on the plan | Some plans may approve for weight loss if criteria are met |
Members can contact Aetna directly or review their benefits online. Aetna aims to support your journey to better health.

Credit: diatribe.org
Ozempic: What It Is And How It Works
Ozempic, a name popping up in weight loss conversations, wonders many. It’s a medication known for its role in managing type 2 diabetes. But buzz about its use for shedding pounds has caught attention. This post dives to uncover Ozempic’s nature and its functioning.
The Science Behind Ozempic
At its core, Ozempic’s active ingredient is semaglutide. It acts similar to a hormone in our body called GLP-1. GLP-1 helps control blood sugar and digestion. Ozempic boosts this action. The results? Lower blood sugar and a feeling of fullness.
- Ozempic slows stomach emptying
- It reduces appetite
- Blood sugar levels drop
Fda Approval For Weight Loss
Once only used for diabetes, Ozempic now has the FDA’s nod for weight loss too. FDA approvals matter. They mean a drug is both safe and effective for its intended use. For weight management, Ozempic went through rigorous tests. The decision: it can help adults with obesity or excess weight.
| Approval Criteria | Outcome for Ozempic |
|---|---|
| Safety | Passed |
| Effectiveness | Confirmed |
Aetna’s Prescription Coverage Policies
When it comes to managing healthcare costs, understanding your insurance provider’s policies is crucial. Aetna’s prescription coverage policies determine whether medications like Ozempic for weight loss receive coverage. Aetna’s decisions rely on their formulary and specific coverage criteria.
Understanding The Formulary
Aetna’s formulary is a list of approved medications. This list shows which drugs Aetna covers. Medications fall into different tiers. Each tier has a cost associated with it. Lower tiers usually cost less. More expensive drugs are higher up on the list.
Here’s how Aetna’s drug tiers work:
- Tier 1: Generic medications, lowest co-pay.
- Tier 2: Preferred brand name drugs, moderate co-pay.
- Tier 3: Non-preferred brand name drugs, higher co-pay.
- Specialty Tier: High-cost prescription drugs.
For Ozempic, which tier applies can impact your out-of-pocket cost significantly.
Criteria For Medication Coverage
Aetna reviews medications based on necessity and effectiveness. They use the following criteria to decide on coverage:
| Criteria | Description |
|---|---|
| Medical Necessity | Is the medication crucial for your health? |
| Prescription Standards | Does a doctor prescribe the medicine? |
| Cost-Effectiveness | Is the medication price reasonable? |
| Formulary Inclusion | Is Ozempic on the list? |
Ozempic may require prior authorization. This means your doctor must prove that you need it for weight loss. Only if all conditions are met, Aetna may cover Ozempic. It’s essential to talk to Aetna directly to understand your coverage.
Navigating Insurance For Weight Loss Solutions
Understanding insurance coverage can be tricky, especially for weight loss medication like Ozempic. Some insurance plans may cover Ozempic, yet often for diabetes management rather than weight loss. A thorough evaluation of your Aetna plan is crucial to determine eligibility and cost-effectiveness of weight loss solutions.
Assessing Plan Options
Start by reviewing your Aetna insurance plan. Look at the Summary of Benefits where prescription coverage details live. Not all plans cover weight loss treatments the same. Key points might be hidden in the fine print.
- Check your formulary: A list of covered drugs Aetna provides.
- Identify coverage tiers: These affect your out-of-pocket costs.
- Review restrictions: Some drugs need step therapy or prior authorization.
- Search for exclusions: Certain treatments might not be covered.
The Pre-approval Process
For drugs like Ozempic, a pre-approval, or prior authorization, from Aetna may be necessary. This means your doctor must justify its need for weight loss. They provide clinical information to Aetna to review.
- Contact your doctor: They start the prior authorization process.
- Gather documentation: Medical history and previous weight loss efforts.
- Submit to Aetna: Aetna will review the information for approval.
- Follow up: Check the status of your request regularly for updates.
Aetna’s decision relies on clinical guidelines, treatment efficacy, and your medical necessity. If approved, Aetna will outline the quantity and duration for Ozempic coverage under your plan.
Successful Claims For Ozempic With Aetna
Many people wonder if their insurance covers medications for new purposes. Aetna users interested in Ozempic for weight loss often find themselves asking this very question. Here we explore real-world scenarios where Aetna approved Ozempic, highlighting successful claims.
Case Studies And Testimonials
Ozempic has shown promising results for weight loss, and some Aetna holders have shared their success stories. By collating a series of case studies and testimonials, a clearer picture emerges.
- A patient with Type 2 diabetes received coverage for Ozempic and noted a significant weight loss as a secondary benefit.
- Another engaged with a lifestyle program recommended by Aetna and documented their journey with Ozempic, receiving full coverage.
- An Aetna subscriber submitted detailed medical necessity letters and saw their claim for Ozempic approved, citing its effectiveness for weight management.
All cases reflect Aetna’s approval process’s complexities and the potential for coverage of Ozempic based on individual health profiles and policy specifications.
Strategies To Improve Approval Chances
Knowing the right approach can drastically increase your chances of getting Aetna to cover Ozempic.
- Start by reviewing your policy details closely to understand the criteria for drug coverage.
- Consult with your doctor to provide astrong medical rationale for Ozempic’s role in your weight loss plan.
- Ensure all paperwork, including a Prior Authorization form, is accurately completed and submitted.
- Gather evidence that showcases how Ozempic could be cost-effective for your health in the long run.
Patients have successfully navigated the approval process by being proactive, prepared, and persistent. Implementing these strategies has made a significant difference in securing coverage for Ozempic under Aetna’s plans.
Note: Individual results may vary based on personal health conditions and insurance plan details.
Reasons Behind Insurance Denials
Understanding insurance denials can be as important as knowing your coverage benefits. Sometimes, Aetna might not cover medications like Ozempic for weight loss. Let’s explore the reasons for these denials.
Common Grounds For Rejection
Insurers have rules that they follow when deciding on coverage. Here are some reasons why Aetna might deny coverage for Ozempic:
- Ozempic is not within your plan’s formulary: The drug might not be on the list of medicines that Aetna agrees to pay for.
- Lack of medical necessity: Your doctor must show that Ozempic is needed for your health. Without this evidence, Aetna might not pay for it.
- Weight loss not covered: Some plans do not pay for drugs used just for losing weight.
- Missing information: If your prescription lacks necessary details, Aetna may not approve it.
Appealing Aetna’s Decision
You can challenge Aetna’s denial. This process has specific steps.
- Review your denial letter: It tells you why Aetna did not agree to cover Ozempic.
- Collect information: Get records from your doctor. These should show why you need Ozempic.
- File an appeal: Send your appeal to Aetna. Make sure you do this within the time limit they set.
Don’t give up: You might win your appeal and get Aetna to cover Ozempic for weight loss.
Costs And Considerations Without Coverage
Understanding the financial impact of medications is vital. If Aetna doesn’t cover Ozempic for weight loss, you face certain costs. Getting clarity on these expenses is crucial. It helps prepare for the treatment journey.
Out-of-pocket Expenses For Ozempic
Ozempic comes with a price tag. It’s an important medication for many. Without insurance, costs can be high. You may need to plan for regular expenses. These include the medicine and related medical visits. Don’t forget about monitoring equipment costs as well. Here’s a quick glimpse into typical out-of-pocket expenses:
| Expense Type | Cost Range |
|---|---|
| Ozempic Prescription | $800 – $900/month |
| Doctor’s Visits | $100 – $350/visit |
| Glucose Monitoring | $20 – $100/month |
| Prices vary by pharmacy and dosage. | |
Remember, prices can change. Shop around for the best deal.
Finding Financial Assistance
Help is available if you need it. Many patients need support to afford medications. Look into these options:
- Manufacturer Coupons: Check the Ozempic website.
- Patient Assistance Programs: Non-profits offer aid.
- Discount Cards: Pharmacies have savings cards.
- State Programs: Some states help with prescription costs.
Research these thoroughly. Dedicate time to understanding eligibility. Some have income limits. Others target specific demographics. Persist in finding the right support for you.
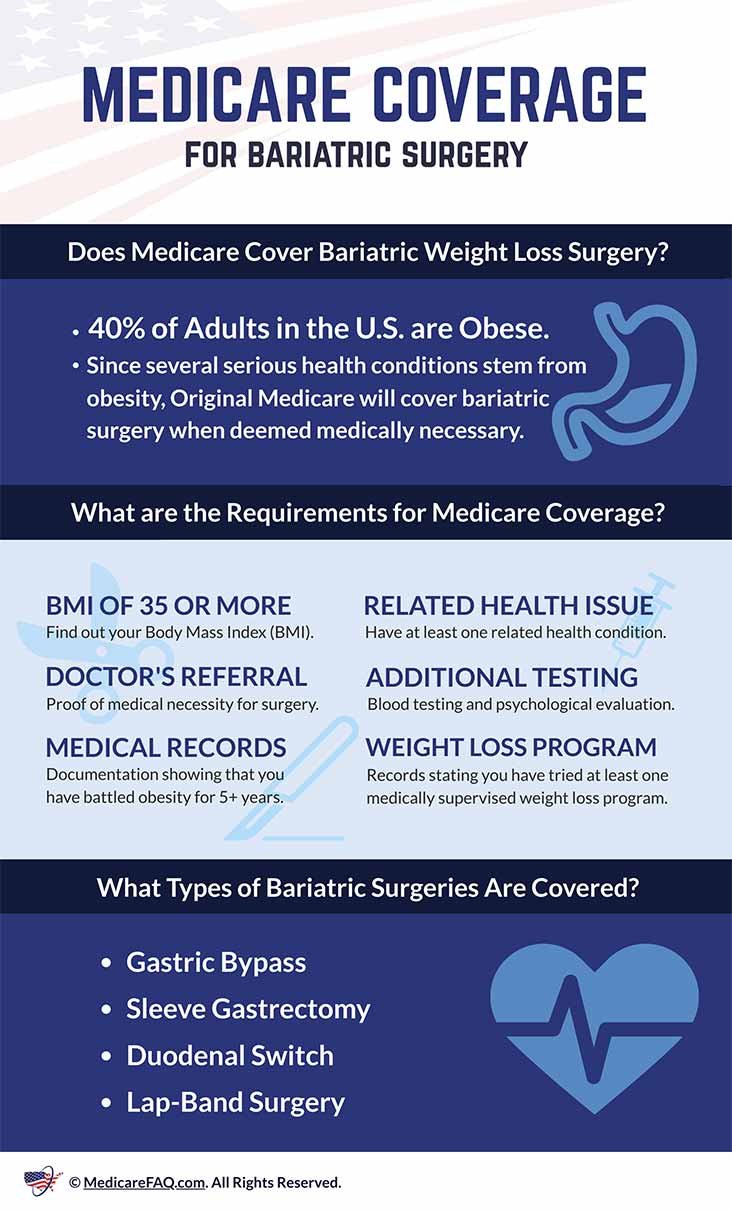
The Future Of Obesity Treatment Coverage
Exciting changes lie ahead in the landscape of obesity treatment coverage. As medical science evolves, insurance providers reassess their coverage policies. Aetna’s coverage for weight loss medications, like Ozempic, is a hot topic for those seeking progressive healthcare solutions.
Emerging Trends In Insurance
Insurance giants are now noticing the long-term benefits of obesity treatment. Recent patterns show a shift towards embracing newer medications. Ozempic, initially used for diabetes, shows promise in weight management. Insurers are now following these trends closely:
- Review of existing policies in light of new clinical evidence.
- Inclusion of weight loss medications on insurance formularies.
- Focus on preventative healthcare measures to reduce future costs.
Aetna and other insurers might soon update their policies to incorporate cutting-edge medications like Ozempic.
Advocacy For Broader Access
Advocates tirelessly work to improve access to obesity treatments. They push for policy changes that could benefit countless individuals. Their tasks include:
- Collaborating with healthcare professionals to highlight the necessity of treatments.
- Urging insurance companies to recognize obesity as a serious health condition.
- Calling for wider coverage of medications like Ozempic, not only for diabetes but for effective weight loss management.
Their efforts suggest a hopeful future where Aetna and similar insurers might extend their coverage to include weight loss drugs for those in need.

Credit: urbanhealthmedia.org
Frequently Asked Questions
Will Aetna Cover Weight Loss Meds?
Aetna may cover weight loss medications if deemed medically necessary and included in your specific plan benefits. Always check your individual plan for coverage details.
Will Insurance Cover Ozempic For Weight Loss?
Insurance coverage for Ozempic specifically for weight loss varies by plan. Patients should check with their provider to determine eligibility, as Ozempic is primarily approved for diabetes treatment.
Does Aetna Medicare Pay For Ozempic?
Aetna Medicare may cover Ozempic if prescribed for a medically necessary condition and if it’s included in your specific plan’s formulary. Always verify coverage with Aetna directly.
Will Aetna Pay For Wegovy?
Aetna may cover Wegovy, but coverage depends on your specific insurance plan and medical necessity. Check with Aetna directly to confirm.
Conclusion
Navigating insurance benefits can be complex, but understanding Aetna’s coverage for Ozempic as a weight loss aid brings clarity. It’s apparent that individual plan details matter greatly. Consult with Aetna directly for personalized information. Taking this step ensures you maximize your benefits while pursuing health goals with Ozempic.
Always verify with your provider for the most accurate coverage updates.